A Look At How Value-Based Care Is Changing The Game
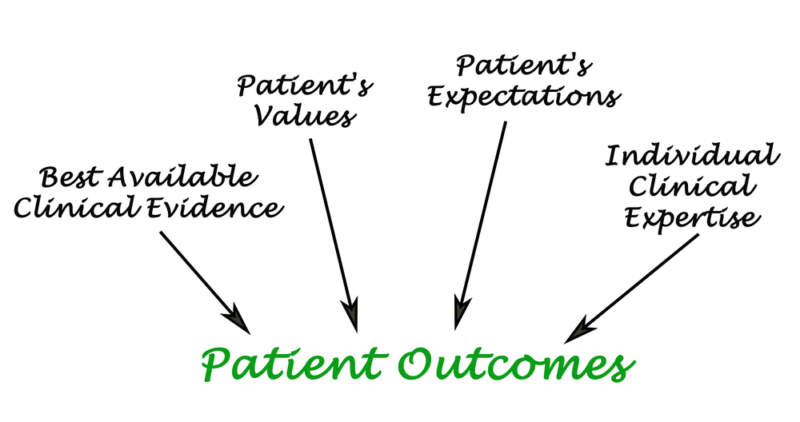
There is a growing trend in medicine that is moving away from fee-for-service health care and towards value-based care. This move is about more than just improving outcomes for patients. It is a way to pull in the rising costs associated with healthcare. It also helps put patients at the forefront of their care, according to many health leaders.
Recently, an entire consortium of experts from major health care companies like Novartis and Kaiser Permanente worked with the health minister from the Netherlands and the Minister of England’s NHS. They called for a whole new approach to care which embraces the patient’s need for attention and that focuses on positive outcomes.
The Difference Value-Based Care Makes
The announcement came with the release of a report from the Boston Consulting Group and The World Economic Forum. The report called “Laying the Foundation for Health System Transformation” has three principles. It discusses measuring costs and outcomes. It focuses on targeted populations and helps customize interventions for these people. It comprises government organizations, medical suppliers, provider, and payers.
The costs of unnecessary tests and treatments are costing the healthcare system up to $50 billion dollars for every $1 billion in revenue. According to the VP of the Advisory Board Company, costs may be a lot higher. Value-based care may help with this, but there are challenges.
“Value” is subjective, and may differ for patients and their providers. It requires metrics to be able to measure care and quality across purchasers, health systems and payers. Organizations must be able to accurately measure costs which is difficult.
CMS and HHS have issued a document that serves as a roadmap for the shift to value-based care. The key to reaching goals is using 21st-century information technology. This allows access to secure data as well as sharing of that data. The 21st Century Cures Act also has provisions that allow for interchangeable operations which prevent EHR vendors from circumventing.
No shocking results have emerged. However, anyone who supports value-based methods agree that more time must pass for effectiveness to show.
Mixed Results
Although the momentum towards value-based care is clear, is there data that supports its benefit with patient outcomes, costs, and engagement?
At The Henry J. Kaiser Family Foundation, Associate Director of the Program on Medicare Policy, Cristina Boccuti says, “Mixed results are being shown by the data. There are initiatives which are returning positive quality and positive savings results while others are more mixed.”
Holly Martin, a senior manager at Top Tier Consulting, agrees. “The fact that people are changing and innovating and viewing results in quality and costs is part of the challenge, and some reduced payments are being seen by Medicare. However, it is hard to consolidate the accumulated learning nationally. Although CMS is happy with the progress and trend, when compared to the overall healthcare spend, the actual dollar amounts which are being saved are really not huge.”
The Hospital Readmission Reduction Program is one positive result. This program was able to lower hospital readmissions, resulting in savings returned to Medicare. Boccuti notes that the program’s success, which penalizes hospitals with elevated thirty-day readmission rates for some conditions, could also be reflected in value-based initiatives from other programs. For example, ACOs (accountable care organizations), to reduce total spending, indirectly have an incentive to lower hospital readmission rates.
Other programs such as the ACOs and medical home model are allowed in use by reducing readmissions and duplicate services, yet not cutting costs.
And although across alternative payment models, the quality of care has remained the same or improved, unless they cut costs they cannot be considered a success. With these models, the goal is to lower costs yet not lower quality or maintain costs while improving quality. The key is for the models that are working to be embraced and for those that are not, they must be abandoned or tweaked, says Boccuti.
Benefits Compound With Experience
At the Healthcare Financial Management Association, director of healthcare finance policy, James Landman explains that experience is also important to consider. “If you look over the data of the biggest of the ACO programs which are under CMS; Medicare Shared Savings Program, you can see the correlation between the time that is spent within the program and ability to generate savings.”
Some of the most successful organizations under programs that are value-based are those who have spent years developing networks that are clinically integrated or working with physician practices and having to deal with global payment contracts that are capitated. He says; “It takes a lot of time to develop those capabilities. When they are developed, you begin to see improvements and traction in quality as well as the efficiency of care.”
For example, he cites, the Comprehensive Primary Care program by CMS. During the first year of the program, it was a struggle for physician practices to even wrap their heads around the program. Several years later, however, there is a positive impact being seen on emergency department utilization and metrics. Care management teams that the practices hired were challenged to drive behavior modification and develop long-term relationships with patients.
Strategies for Value-Based Care Results to Increase
Despite a variety of challenges, there are steps which organizations can take to increase value-care based benefits. Finding the way to stratify patients by risk as well as analyzing and evaluating the data can bring about a reduction in expensive ED use as well as improvement or stabilization of underlying chronic conditions – savings which according to Landman, will be long-term. He says; “Organizations which have placed their focus on this have achieved results that are demonstrable both in reducing the cost of patient’s care as well as improving their conditions.”
However, for this to be done it will require investing in an IT infrastructure which enables predicting modeling and data collection, also in care management professions – traditionally, none of which are paid for, at least not in a manner that is holistic, Landman points out. Under alternative payment models, those resources are now becoming available, therefore organizations can make the investments that are necessary and start performing interventions which will translate to cost and quality gains for the patient population.
Structural adjustments must also be made by organizations in terms of collaborating and partnering on patient care across the continuum, and they must understand their costs as well as which ones are variable or fixed, explains Martin. Close management of margins will be required by any at-risk arrangement or a fixed payment.
Due to the current uncertainty in regards to funding and reimbursement models, providers are encouraged by the Advisory Board to pursue “no regrets” improvement initiatives such as improving access, reducing costs structures, and reducing variability and inefficiencies in care and better aligning with the staff. Reducing unnecessary utilization seems to be in an area in which health systems can make a difference and witness results.
“Eliminating unnecessary utilization, even in hospitals which are on a fee-for-service basis and heavily paid, will positively impact the outcomes and the bottom line”. Johnston explains. “So the focus of our clients is mainly on understanding what drives the variation across the entire episode of care, this includes pre- and post-acute, as well as organizing their clinical leaders and physicians to determine the proper processes and protocols to get rid of variability and optimize outcomes.
Johnston notes that it is also key to focus in specific disease states, as well getting those huge stakeholders in the health system to the table so that change can be discussed and implemented.
Moving the Needle
Despite an interest that is growing as far as value-based payment models are concerned, they still account for a percentage of overall healthcare costs that is not very large. Most organizations are mainly fee-for-service, although there are many which are experimenting with care that is value-based as well as building the capabilities which will be needed as more payers – commercial and government – reward care and lower costs that are evidence-based.
Landman explains; “The point where we are at is one where I do not believe that we necessarily have the penetration of the depth of value-based payment which is what will actually turn the ship. There is, however, a log of organizations that are hard at work developing what they believe they will need to have in place when the ship actually turns.”
“What providers must realize is that initiatives that are value-based are in both the commercial market and Medicare,” says Boccuti. The challenge here is to see where they can achieve alignment on payers, as well as how those will align with Medicare.
Call us or contact Progressus Revenue for more information about our medical billing strategies, practice management solutions and ancillary care programs.